Meet the Doctors & Staff
Gavin J. Green, DDS, Gavin H. Green, DMD, and our experienced and friendly staff specialize in maintaining your dental health and helping you improve your appearance.
Meet Dr. Gavin J. GreenMeet Dr. Gavin H. GreenSuresmile®
Suresmile® digital orthodontic technology uses clear aligners and a sophisticated treatment plan to move your teeth more efficiently than ever.
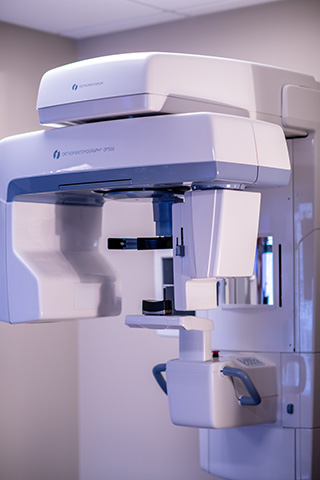
Intraoral Scanner
Our intraoral scanner captures a direct optical impression, which then produces a 3D model. No more gooey alginate impressions!
Family Dentistry
From preventive care and minor restorative therapy to cosmetic treatments, we’re here for your family’s dental needs.
Pediatric Dentistry
We love seeing children in our office and usually recommend the first visit around age 3.
Cosmetic Dentistry
The ultimate goal of cosmetic dentistry is to restore a beautiful smile and keep it healthy for years to come.
Emergency Dental Care
Our goal is to help you to minimize the risk of emergency treatment, but if an emergency occurs, we’re here to help.
Welcome To Green Dental
Looking for comfortable, confident, and convenient care from dentists in Glenview? You’ve come to the right place. From the minute you walk into our office, you will notice a difference at Green Dental. We care about you, your family and your friends, and we’re here to help you achieve your healthiest, brightest smile.
At Green Dental, we know every person’s dental needs are unique. That’s why we offer a comprehensive selection of treatment options in a state of the art atmosphere. We're confident we can provide superior service that no other dentist in the greater Chicagoland area can offer.
We specialize in improving smiles with gentle dental care, including:
We take great pride in keeping your smile beautiful. Our promise to you is that the treatments we create will look as good as or better than the teeth nature gave you. And to make sure we keep that promise, the products we recommend and use are the absolute highest quality. You can trust your smile with us.
Discover a new dental experience at Green Dentistry in Glenview, IL! We look forward to caring for you and your family’s dental needs.











 Website Powered by Sesame 24-7™
Website Powered by Sesame 24-7™